What is Health About?
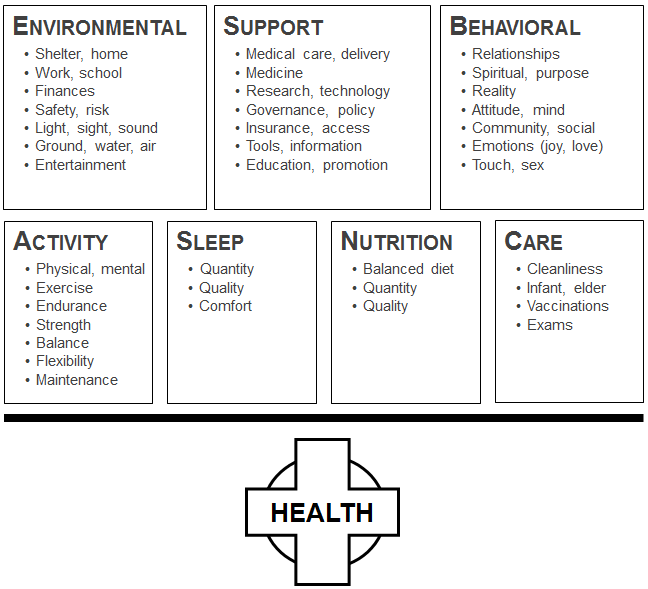
Our health is a combination of several key things that need to stay in balance in order to remain healthy. We need to feed our bodies, we need to flex our bodies, we need to rest our bodies, and we need to manage the external forces that affect us. If we are out of balance, chronic diseases and other disorders may occur.
There are 7 components to health and to be healthy, all 7 must be in balance.
How far out of balance are we?
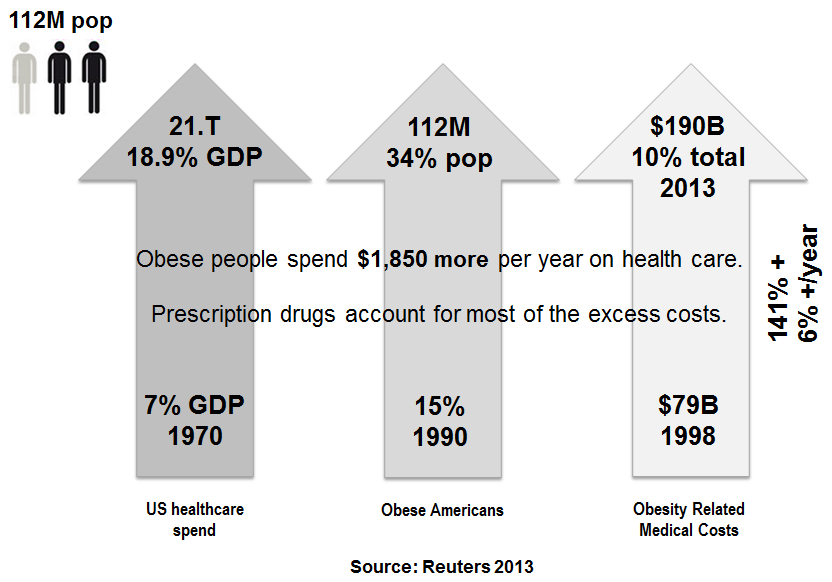
Sometimes tough facts are difficult to swallow, but denial is no longer an option. Let’s take a look at two chronic diseases, obesity and diabetes. About 1 in three people are obese in America. The alarming statistic is the increase from 15% of the population in 1990 to 34% in 2013. The figure rises 6% year over year. A study in 2010 by the Organization for Economic Cooperation and Development (OECD) said 75% of Americans will be overweight by 2020. Obesity is responsible for 5-10% of total health expenditures in the United States. An obese person incurs 25% higher health expenditures than a person of normal weight in any given year. In the United States, obese people are 76% more likely to suffer short-term disability adding production losses to health care costs that account for over 1% of the GDP. The costs will rise as obesity related diseases develop. A Johns Hopkins University researcher claims, in the 2008 journal Obesity that about 65% of Americans will be overweight by 2030. Costs to treat obesity and health related costs could also rise at staggering amounts. Our economy may not be able to support those increased costs.
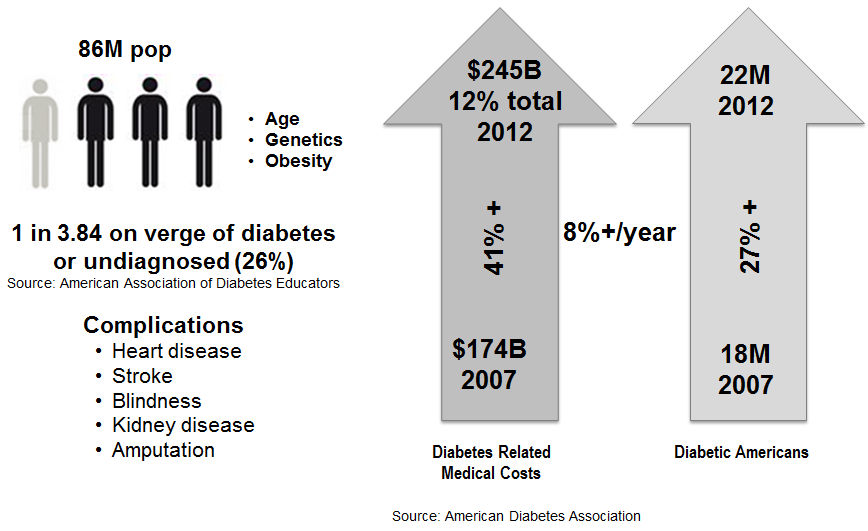
If we look at diabetes, about 7% of the population has been diagnosed with diabetes. The alarming facts is about 26% of Americans are on the verge of diabetes or undiagnosed. Complications due to diabetes lead to more serious diseases such that the related costs are $245 billion in 2012. According to the CDC, 1 in 3 adults could have diabetes by 2050 if current trends continue. The International Diabetes Federation predicts as many as 438 million people in the world will have diabetes by 2030.
The trends in both diseases are similar and growing at high rates. How we address chronic diseases in people requires immediate attention if we are to manage medical costs and the population’s health.
Excerpted from my book titled, “Commercializing Consumer Engagement.”