2006
Smart card technology used to advance the traditional medical insurance card into a multipurpose card so to assist in access, registration and payment for members. Not only does it combine three existing insurance cards (medical, dental, drug), it can store relevant personal information.
Industry Situation
Industry and Technology Convergence
The convergence produces a sweet spot of opportunity to many industries. Each industry will gain entry into this new market because of the expanded opportunities. This may cause confusion by the consumer as to which card to acquire.
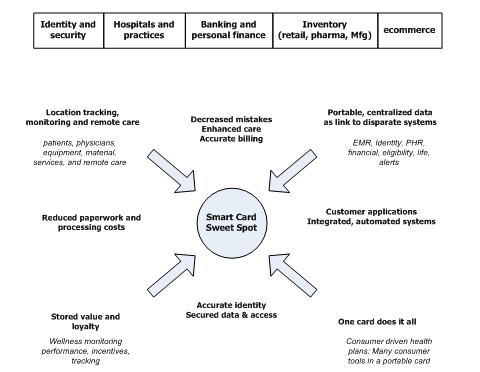
Figure 1 – Convergence and the Sweet Spot
Vendors with the most complete and attractive offer may win the minds of the consumer. Since consumers are also happy to cut down on the number of cards in their possession, a single card to perform multiple functions is desirable. Many businesses are aiming toward a single card to perform multiple functions to cut costs and to increase revenue opportunities. Cards with added capabilities will provide vendors the ability to sell real estate on their card for additional revenue streams. New services can be offered by the card provider to further increase revenue.
Analysis based on observations
Europe is ahead of US based smart card deployment in the health care sector by 2 to 3 years. We can gain insight by reviewing their progress and doing it better. European solutions focus on identity, demographics, and PHR data.
There have been attempts to pilot smart cards for debit transactions and health ID in the US since 2003/2004. Typically smart cards in the health care sector have focused on financial transaction processing or ID/health plan/medical data applications or both. There is no evidence that a vendor or health provider is looking at a complete solution set covering financial transactions, PHR, EMR, wellness tracking, and life management. A complete solution including wellness tracking, identification, scheduling, location tracking, and a portable PHR would provide United with a differentiator.
Smart cards offer the most secure access, transaction processing, and data storage over other technologies. Smart cards and supporting applications move closer to removing paper from transactions. Using a reliable, secure medium such as smart cards, helps to reduce identification mistakes, reduce medical errors, reduce redundant tests, increase information availability and sharing among medical professionals, and reduce billing errors. Adding biometric data decreases mistakes in identity and fraud.
Hospitals, clinics, and large practices already equipped with smart card systems pose another dilemma. United needs to acquire real estate on the smart cards and in-house systems so United can provide our required services. Without standards in the industry, alliances must be made to ensure usability and interoperability over a large customer base and set of applications and services.
Active RFID seems to be the favored technology in the health care sector with the greatest return, but privacy, standards, and adoption issues exist at present. These early adoption issues will dissipate as the benefits of that technology and solutions surface.
Pilot
Considerations
Some smart card pilot candidates use a combination of magnetic stripe, contact microchips, and active RFID. From the research and observations below, a hybrid card will allow health care providers to use the card across multiple card processing systems since one card type may not fit all systems in use at health care providers. If United adopts the hybrid mode of reading and accessing multiple smart card technologies, we gain an advantage as the common data point for all health smart cards. This approach is more costly.
The technology of choice should be one that enables all present specified services and allows for expansion to evolve to more advanced solutions if United wishes to keep the card in the field for many years to gain maximum value from card deployment. To provide the right solution supporting standard requirements for smart cards across United, a list of services needs to be gathered and assessed as the first step. The recommendation for standard requirements should account for the company strategy, service requirements, health care provider requirements, and pilot partner limitations and requirements. If we use the vendor funded method for a pilot, much will be determined by the vendor and their relationship with the health care providers. If we use a United funded method for the pilot, we have more control on the pilot requirements.
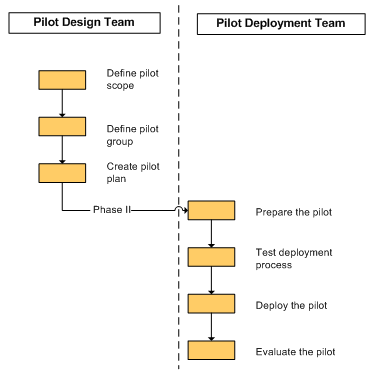
Pilot Approach
Pilot planning is split into two sections. The first is the design stage that organizes all aspects of the pilot and provides a baseline for understanding to all pilot participants. The second is the deployment stage that executes on the design resulting in a carefully controlled pilot.
Phase I Design
- Define pilot scope
- Define the pilot group
- Create the pilot plan
Phase II Deployment
- Prepare the pilot
- Test the deployment process
- Deploy and test the pilot
- Evaluate the pilot
Figure 2 – Pilot planning diagram
The Pilot Scope
Key Objectives
Manage a small pilot sample that will be discreet and operate under a low profile. Choose a progressive hospital with a track record for adopting new processes and technologies to ensure maximum success.
- Identify problems, opportunities, processes, and issues moving to smart card use.
- Understand issues: of adoption, accuracy, privacy, automatic, and simplified transactions
- Understand technical issues of available technologies, systems, security, information transfer, network processing, data extraction, access mechanisms
- Fortify UnitedHealth Group’s position as an innovative leader.
Exante’s direction, objectives, and expectations
Exante direction: To be a dominant leader in financial health accounts for UHG and non-UHG payers with a 30% market share by 2009.
- Create a standardized smart card offer for United
- Support the following applications and services:
- HSA debit transaction processing (?)
- Eligibility applications using a smart card (?)
- Access to basic PHR data (?)
- MasterCard credit line (?)
- Fold into the Integrated Card Project (?)
United’s Value to Employers and Healthcare Providers
Value and benefits are determined by the services offered to customers. By offering financial transaction services, identity services, and basic PHR services, the following benefits can be realized:
- Single card solution to eliminate confusion and reduce card costs
- Accurate consumer identification at patient care areas
- Faster check in/out for enhanced consumer experience
- Less mistakes in consumer information and records
- Reduction of medical errors due to more accurate information that is delivered faster
- Accurate billing and care with accessible eligibility information
Requirements to move forward
Create and lock down on the pilot’s objectives, expectations, funding, and features.
Secure funding for pilot
- Option 1: (preferred) Internally driven pilot and identify customer base willing to contribute
- Option 2: Vendor driven pilot that best aligns to United’s objectives
- Option 3: Fold in Integrated Card pilot since it is funded and choose a customer base with features aligned to United’s direction
Secure resources to work the pilot planning, development, deployment, and evaluation
- Smart Card solution vendor(s)
- Willing consumers/employers
- Exante FS support
- UT support for integrating into backend systems, portals, and applications
- Innovation Lab support
- Pilot expectations
Identify pilot participant opportunities and contact information
- Siemens and Mt Sinai (?)
- IBM and BellSouth (?)
- IBM internal unified card (?)
- Integrated card project (?)
- BellSouth (?)
- Parco and MedStar (?)
Competitive and Launch Observations
Visa, Blue Cross and Blue Shield to offer health debit cards
Visa and the Blue Cross and Blue Shield Association are partnering to offer a co-branded health debit card for health related costs.[1]
German companies to test electronic health cards
A German health care and insurance group and T-systems international GmbH, the IT services arm of Deutsche Telekom AG, on Monday launched a pilot to test electronic health cards once year before the German government’s mandate to introduce the technology. T-Systems and Bundesknappschaft hope to provide electronic cards to 20,000 patients and 75 physicians in the first quarter of 2006.[2]
Germany to issue electronic health cards
The German government has announced that it will begin issuing electronic health cards by January 2006 to customers of every health insurer in the country, the BMJ reports. The health ministry expects the system to improve efficiency and save up to $1.7 billion in three years.
The patient information on Germany’s health card will come in two parts. The administrative part contains data on patients’ insurance status, their rights to be treated abroad and their prescriptions. The optional medical part contains only information that patients approve, such as drugs they take, emergency data, previous operations or their personal health documentation.[3]
Europe launches Smart Cards
Thirteen European countries last week introduced smart cards to replace the paper-based reciprocal health agreements used to provide citizens’ health insurance and personal information when they travel to other member countries, E-Health Insider reports. The European Health Insurance Cards contain chips that connect to a server in the cardholder’s home country.
The server will store information such as name, address and next-of-kin. Basic medical information may also be included. For emergency purposes, contact information will be displayed on the front of the card. The cards should reduce costs and provide easy, equal treatment in participating member countries, according to the Netc@rds Consortium, which is managing the initiative (E-Health Insider, 6/1).
Currently, citizens of EU nations must travel with an E-111 document, which verifies that the holder is entitled to free or reduced-cost emergency medical treatment in EU member states (iHealthBeat, 2/3).
The 13 initial countries include Belgium, Ireland, Spain, Estonia and Slovenia. The United Kingdom will join in 18 months, when it stops using paper forms. The United Kingdom plans to begin working on proposals to integrate the cards with its national IT project. The European Union hopes to have 167 million cards in circulation by 2006.[4]
Pennsylvania health system to offer online registration, smart cards to members
A Pennsylvania health system this summer will begin piloting an online scheduling system that lets patients pre-register for lab tests, outpatient surgery and radiology appointments, and standard physician appointments. Heritage Valley Health System is introducing the system as part of a $40 million, eight-year plan that the system initiated in 1997, with the ultimate goal of being “completely wired” by 2005, according to CEO Norman Mitry. Heritage Valley also plans to expand a smart card program by issuing “Care Cards,” which will facilitate online access to patients’ medical information, to the system’s 100,000 customers next year. Approximately 7,000 Heritage Valley employees and their dependents began using the cards in January. The cards will let patients register for appointments and procedures at self-service kiosks that will be installed next year in registration areas at the system’s hospitals and in waiting rooms at physician offices.
Use of the smart cards and kiosks will eliminate the need for patients to complete about four pages of paperwork before each appointment. Health system officials expect the project to ease the workload for registration clerks and streamline administrative functions throughout the system.
Heritage Valley has spent approximately $1 million on the online scheduling system, and officials anticipate spending $3 million to $5 million more on the kiosks and the smart cards. Heritage Valley Health System is a two-hospital health system that includes 40 physician offices and 15 satellite clinics.[5]
Health information card project moves forward in Nebraska
Several Nebraska hospitals will install software to read smart cards that store patients’ medical information and can be accessed by a handheld computer, the Omaha World-Herald reports. The Health Data Card could be used to access a patient’s identification, basic medical history, insurance, allergies and the names and numbers of a person’s doctor and emergency contacts.
The retail price of the card is $65 to $75, but large groups could pay less than $30 each. The company is talking to insurance companies, employers and other groups and hopes to issue 100,000 cards in the next year, the World-Herald reports. HDC is distributing the software to medical providers for free, which will be covered by revenue from the card sales, said Dr. Daniel Dietrich, one of the company’s founders. The card-reading devices cost about $30 to $50.
The success of the cards will depend on getting them in circulation and making them worthwhile for providers, patients and insurers, said Robin Kammandel, executive director of the Metropolitan Omaha Medical Society. Doctor’s offices may not have time to sell the cards to patients, and it is unclear whether insurers, employers or consumers will buy them, Kammandel said.
Dietrich came up with the idea for the card based, in part, on his experiences as a patient. Dietrich said he continually had to repeat his medical information to providers, and once forgot to mention his penicillin allergy when he was groggy with medication. He tested the system by giving cards to his patients and placing card readers with other physicians.[6]
Cool reception for VeriChip reflects hospitals’ concerns about smart cards
While smart cards have been used for “more than a decade” in Europe to store patients’ personal and medical information, American hospitals have been more reluctant to adopt similar technologies, the Palm Beach Post reports. The latest company to encounter a cool reception from hospitals is Applied Digital Solutions, the maker of the VeriChip implantable microchip, which stores an identification number that providers can use to access a patient’s medical records online. As with smart cards, hospitals say they are concerned about the costs and potential liability issues associated with the technology.
Applied Digital implanted the VeriChip in eight people last week and says it has a waiting list of thousands who want the device. But even in Palm Beach, Fla., where Applied Digital is based, none of the major hospitals has yet acquired the handheld scanners that are needed to read the information stored on the chip.
In an attempt to spur adoption of the technology, Applied Digital initially is offering the scanners to hospitals in Palm Beach and Broward counties for free, although the devices later will be sold for about $1,500. Company officials will be meeting with hospital leaders across the next month to try to convince them that the application could save patient lives. Hospital officials, however, say one of their chief concerns is ensuring that information stored on the chips—or in the online database—is accurate and up-to-date and remains confidential.
Those are the same concerns that have limited use of smart cards, according to Ed Donaldson, who founded smart card vendor Linc International in 1996. The company folded after three years of attempting to market its products to hospitals. “A physician is still hesitant to accept information when they don’t know who entered the information and where it came from,” Donaldson said.[7]
GAO report considers federal smart card programs
Government agencies deploying smart card technology need to address personnel and technical challenges to realize the full potential of the application, according to a report from the General Accounting Office. Agencies such as the Department of Veterans Affairs and HHS have piloted smart card technology for a variety of projects, including storage of health information and processing health benefits.
The report looks at a VA program launched in April 2001 that stored beneficiaries’ medical and personal information on smart cards as part of a project intended to expedite patient registration at VA hospitals. Although VA officials credited the cards with reducing registration times by 45 minutes on average, they did not expand the program beyond its original two pilot locations because of budget constraints and problems integrating legacy computer systems throughout the VA health system.[8]
EU to research wearable health monitors
The European Union is in the final stages of negotiating a $16 million research effort to develop wearable health monitors, which could expand health care coverage and decrease the cost of monitoring conditions such as diabetes, cardiac problems, high-risk pregnancies and stress, Electronic Engineering Times reports. At a conference in Cancun, Mexico, last week, as many as 17 papers detailed these and other prototype systems using handheld devices, low-power sensors and wireless networks.
The European Commission is working with private companies on three future projects—a cardiac monitoring system from Philips, a sensor “garment” from Italian company Smartex and a mask that detects neural stress based on facial expressions.
Philips’ My Heart system will be used to monitor, diagnose and treat heart conditions such as arrhythmia. The 45-month project could begin in January and includes a group of electronics, medical and textile companies, said Josef Lauter, a principal scientist at Philips Research. The Smartex project will follow up on the company’s Wealthy system, a wearable garment that contains sensors and electrodes knitted into traditional materials. The Wealthy system is not expected to be used commercially, but the next stage of the product will contribute to the EC’s initiative, according to Smartex’s Rita Paradiso.
Ericsson created its MobiHealth system based on a personal digital assistant that links to sensor networks on the body and communicates with physicians through cellular networks. A three-month project will track about 25 patients with a variety of conditions and should be completed in February.
While it’s difficult to predict the growth of wearable health-monitoring systems, research into the systems will be “exponential” during the next five years, according to Paolo Bonato, director of the motion analysis lab at Harvard Medical School’s Spaulding Rehabilitation Hospital.[9]
Georgia Physician Network Tests Ambulatory EMRs
Blue Cross Blue Shield of Georgia and the Piedmont Clinic, an Atlanta physician network, are evaluating an ambulatory electronic medical records system for clinic medical offices and health plans. While EMRs have been expensive, difficult to use and have lacked a standard clinical vocabulary, the technology can reduce duplicative testing and provide clinical reminders for patient care, according to a BCBSGA press release.
Piedmont and BCBSGA have hired health information consulting firm JHD Group to conduct an evaluation study and develop the business case for the records system. The evaluation should be complete early this year.
The Piedmont Clinic is a 444-member physician group and a subsidiary of the not-for-profit Piedmont Medical Center, which includes Piedmont Hospital.[10]
WSJ Examines Increased Use of Telemedicine To Reduce Costs
The Wall Street Journal on Thursday examined how telemedicine has begun to move “into the policy mainstream” as governments and technology companies are “investing heavily to tap its potential for sharply reducing health care costs for a growing elderly population.”
Telemedicine, which first became available in the 1970s, allows physicians to read the electrocardiograms, blood pressure levels and X-rays of patients from remote locations. Worldwide, Netherlands-based Philips Electronics, France-based Alcatel and Italy-based Telecom Italia have launched telemedicine ventures. In the U.S., the Department of Veterans Affairs has begun to use telemedicine in some VA health care facilities, and Blue Cross of California in January plans to expand the use of technology to reach 90,000 members of the California Public Employees’ Retirement System who live in rural areas.
The advantages of telemedicine “are commanding increased attention,” but the technology also has “limitations,” the Journal reports. According to the Journal, a “remote visit can deprive doctors of the subtle cues they often pick up when seeing a patient in person”.[11]
Card Reader To Give Patients Instant Copayment Information
BlueCross BlueShield of South Carolina is offering physicians a card reader that will allow patients to use issued cards to find out instantly how much they owe and how much the insurer will pay, the Wall Street Journal reports. The reader, which is manufactured by Companion Technologies, is being introduced at a time when patients are being asked to cover a growing proportion of their medical bills, the Journal notes.
As part of the plan, all BCBS patients will be able to swipe their through the device, which will use broadband Internet access to communicate with the insurer. In addition to providing payment information, the card reader also will be equipped to process credit and debit card payments. Companion Technologies is expected to start marketing the device in August for a monthly lease price of $19.95, and BCBS officials say they will distribute cards to members over the next year.
According to Harvey Galloway, president of Companion Technologies, “the benefit to the doctor’s office is knowing, while they have the patient in front of them, how much the patient liability is, and not having to go after them after they leave the office.” The Journal notes, however, that some claims might slow down if there is no referral on record or if there are other complicating factors that require somebody at BCBC to sort through the claim.
Katy Henrickson, a senior analyst at Forrester Research, said several companies are developing similar products to speed up the payment process.[12]
N.Y. Hospitals Speed Registration with Cards, Online Options
University Hospital in Syracuse, N.Y., last week began issuing special cards to patients who register before coming to the hospital in an effort to cut wait times, the Syracuse Post-Standard reports. Other Syracuse hospitals are adding online registration services to expedite the check-in process.
At University Hospital, patients registered for certain elective or other scheduled procedures present a SpeedPAS card at the registration desk, where they receive their complete paperwork and are sent to the appropriate department. One week before an appointment. Patients receive a letter containing a SpeedPAS card and asking them to call the hospital and register. Once they register by phone, patients are given a number to write on their card. The SpeedPAS initially will only be given to patients coming in for services in certain departments. Hospital officials expect to issue the cards to nearly all pre-registered patients by the end of the summer.
St. Joseph’s Hospital Health Center recently began letting patients register online or by phone. Once they arrive at the hospital, patients can go directly to the department where they have an appointment. The online system reduces the amount of “phone tag” involved in the process, according to the hospital. Crouse Hospital also plans to begin an online pre-registration service.[13]
California Government Proposal Includes Smart Cards to Prevent Fraud
A proposal to fingerprint and supply California’s Medi-Cal patients with computerized cards to prevent fraud is one of a few “controversial” proposals in Gov. Arnold Schwarzenegger’s (R) plan to reform state government, the San Jose Mercury News reports.
Medi-Cal is the state’s health care program for low-income residents. The California Performance Review would increase Schwarzenegger’s authority, create 11 new agencies and eliminate 118 boards or commissions in an effort to streamline the government and save the state an estimated $32 billion in the next five years (Feder Ostrov, San Jose Mercury News, 8/5). Among other information technology-related proposals, the plan calls for California to:
- Develop an online state child immunization registry (Hubbell, San Francisco Chronicle, 8/4); and
- Combine the eligibility requirements for the state’s low-income assistance, Medicaid and food-stamp programs and move them online (iHealthBeat, 8/4). The move is expected to save the state money by coordinating health care data that is stored in 60 different information systems, the Mercury News reports.
Other potentially controversial proposals involve eliminating an independent state HMO watchdog agency and identifying HIV patients by name to state public health authorities. State Sen. Deborah Ortiz (D) said lawmakers would review the governor’s plan. “… Unless we provide more money to the system, efficiencies are not going to result in more favorable outcomes for Californians,” Ortiz said.[14]
Atlanta Physicians Will Pilot Health Credit Cards
Atlanta will test a credit-card machine that will allow physicians to access information about a patient’s health benefits by swiping a card and then printing out the information, the Atlanta Business Chronicle reports. Financial transaction company First Data will launch the pilot in January.
The company is not the first to pilot such a project. Wyoming, North Dakota and Nevada have programs that use “smart cards” to store medical records, the Chronicle reports. First Data’s rival HealthTransaction Network also is encouraging insurance companies to issue debit cards that would connect to medical spending accounts.
First Data’s machine, made by Hypercom, will feature smart-chip technology and magnetic strips. The chips are not being tested in the pilot, but they allow more information to be transmitted and stored, the Chronicle reports. Once some privacy issues are resolved, the terminals will include the chips, which already have been used in Europe, said Beverly Kennedy, president of First Data’s health care division. The machines will plug into walls like credit-card terminals and will be easy to use, she said.
To minimize the risk for physicians, First Data will provide the terminals at no cost but will still collect transaction fees since it owns the network that carries the data, the Chronicle reports. The terminals will first be tested in doctors’ offices and will offer only eligibility data. Insurance companies taking part in the program will issue their customers special cards for use at participating health care facilities. Blue Cross Blue Shield of Georgia, one of the largest insurers in the state, might participate, the Chronicle reports.
Officials plan to eventually broaden the program on a national level to opticians and dentists and to offer comprehensive medical information including referrals, authorization and claims status. They also hope the system will cut health care administration costs, which stand at $275 billion a year.[15]
Athens Public Transport Employees Get Electronic Health Cards
Employees of Attika Metro System, the underground railway system in Athens, Greece, have been issued electronic health identification cards to help ensure their safety during the Olympics, E-Health Insider reports. The Global Health ID card contains a patient’s next-of-kin information, medical information such as allergies and blood type, and insurance and medical contact information. Details about inoculations and operations can also be added.
Each patient has an ID number, which they use to access their medical information online. Patients enter their medical information in a series of templates, and they are responsible for keeping their records current. The online record is accessible only through the card, and the information is deleted if someone reports a missing card.
Every emergency department in Athens is wired with encrypted Internet connections, an extra feature added for the Olympics so that patient record templates can be translated and edited into Greek. Clinicians can also update the record and upload information such as X-ray results. Emergency services could eventually access the information through a personal digital assistant with a wireless Internet connection, said Les Parsonson, managing director of PEMMS International, which developed the card system with Alliance Security International.
There have been “overwhelming requests” for the cards from other Metro systems throughout the world, said Steven Baker, CEO of Alliance Security. The company is also working with travel insurance companies and private medical firms. Individuals can purchase a one-year subscription to the service for $18.[16]
Study: Health Care Organizations Prefer Active RFID to Passive RFID
A recent study found that health care organizations prefer active radio frequency identification technology to passive RFID technology, which often is used in retail warehouses, Healthcare IT News reports.
The “Healthcare Without Bonds: Trends in RFID” study, conducted by Spyglass Consulting Group, found that passive RFID technology accounts for less than 23% of all RFID applications implemented by health care organizations. In passive RFID systems, a reader must be waved next to a transponder with an RFID chip, while in active RFID systems, signals constantly are transmitted between transponders and transceivers, Healthcare IT News reports.
“Passive RFID is not ready for primetime,” said Gregg Malkary, founder and managing director of Spyglass Consulting. Spyglass, which interviewed more than 100 health care organization professionals for the study, found that lack of industrywide standards, less-expensive strategies such as barcoding, and a lack of government or regulatory mandates deter the implementation of passive RFID technology.[17]
RFID Technology Could Assist in Emergency Response Efforts, Bloomberg News Reporter Says in WTOP Radio Interview
WTOP Radio’s “WTOP News” on Tuesday included an interview with Fred Fishkin, Bloomberg News technology reporter, about the limits of IT in responding to a national disaster such as Hurricane Katrina and which new technologies could be useful in a future crisis. According to Fishkin, technology and new forms of communication “may not be available” when public infrastructures are completely destroyed. However, Fishkin said that radio frequency identification technology “has some potential” to assist in a future disaster. RFIDs on wrist bands could track people as they are moved from place to place after an emergency, Fishkin said (“WTOP News,” WTOP Radio, 9/6).
Related Commentary
As the flood waters from Hurricane Katrina recede, “a woefully inadequate medical care system for the poor,” which has failed New Orleans and “most other [U.S. cities] for decades” will be exposed, Jonathan Weiner, professor and deputy director of the Health Services Research and Development Center at the Johns Hopkins University Bloomberg School of Public Health, said on Monday in a commentary on APM’s “Marketplace.” According to Weiner, public health agencies should develop a “medical Marshall Plan” for the country, including rebuilding clinics and hospitals “so that they are better than they were before” as part of a “comprehensive network” featuring universal access to care, prevention and recognition of social health factors. However, private health care providers can not “re-engineer the system piecemeal” and will require assistance from the federal government by redirecting some of the $2 trillion health care budget to improving public health infrastructure.[18]
Former HHS Secretary To Publish RFID Proposal
Former HHS Secretary Tommy Thompson in the next 50 days plans to publish a proposal for widespread implementation of implanted radio frequency identification chips, Red Nova/The Business reports.
The RFID chips would hold individuals’ medical records and would be connected to a national health IT network. Thompson – who now is a director at Applied Digital Solutions, the maker of the chips – had a VeriChip inserted in his own arm.
VeriChip spokesperson John Procter said “virtually everyone” would benefit from RFID chips, which would cost about $200 per person, but civil liberties groups have expressed privacy and security concerns over RFID chip implantation.[19]
Calif. Act To Limit RFID Faces Setback
The California Assembly Appropriations Committee on Thursday put on hold for the year a measure that would limit public agencies’ use of radio frequency identification devices, the San Jose Mercury News reports. State Sen. Joe Simitian (D), who introduced the bill, has pledged to try to revive it before the Legislature adjourns on Sept. 9.
The Identity Information Protection Act of 2005 (SB 682) would prohibit skimming or theft of information on RFID devices, require the state to include strong security protection and encryption of personal data in any future use of the technology, and establish a three-year moratorium for expanding the technology, the Mercury News reports. The act, which was “shelved” without discussion, aimed to address the threat of personal privacy and tracking if RFID chips were implanted in driver’s licenses, school IDs, government health benefit cards and public library cards.
The legislation, which the state Senate has approved, is supported by the American Civil Liberties Union, the Electronic Frontier Foundation and the Privacy Rights Clearinghouse.[20]
iHealthBeat Rounds Up Coverage On RFID Privacy Concerns
The FDA last week approved the use of the VeriChip, a radio frequency microchip planted under the skin that stores patients’ medical information. The Applied Digital Solutions chip, about the size of a grain of rice, contains a code that physicians can scan to retrieve information, such as patients’ allergies and prior treatments (iHealthBeat, 10/14).
Several publications recently addressed the privacy concerns surrounding RFID technology. Summaries of the articles appear below:
eWeek: The RFID chip from Applied Digital Solutions has “kicked up a media furor over potential privacy concerns,” eWeek reports. Because the chip contains identification numbers that provide access to medical records, the number could potentially let anyone access health records, eWeek reports. A unique identifier, which is not currently part of the national electronic medical record plan, could be used to obtain a patient’s complete and correct medical information, according to the article.
“There’s more controversy than there needs to be,” said Mark Leavitt, medical director at the Healthcare Information and Management Systems Society. “It’s just a higher-tech version of the medical ID bracelet.” There also is concern among analysts that the chip is not very useful and “may simply serve to further muddy the health IT debate without offering much of a contribution,” according to eWeek (Lawrence, eWeek, 10/15).
In an eWeek opinion piece, contributing editor and emergency medical technician David Coursey writes that RFID technology could primarily benefit patients in some cases by tagging medical devices and surgical instruments and “only secondarily” by providing patient identification. RFID chips could help identify Alzheimers patients or those with chronic conditions by providing an ID number and a primary diagnosis to aid emergency workers, Coursey writes. Although there are many civil liberties issues involved with such tags, in each case either the patient or legal guardian would decide whether to implant the RFID tag. “Medical RFID is only for the patients who need it,” Coursey writes. “But like so many other medical technologies, it can save lives when used properly” (Coursey, eWeek, 10/15).
InformationWeek: While the “upside” of RFID technology is “immediately apparent to those involved in health care,” privacy concerns remain, according to InformationWeek. “[T]he general public already is skittish about the privacy questions around RFID, and just the mention of RFID implants gives most people the heebie-jeebies,” according to InformationWeek (Soat, InformationWeek, 10/18).
BBC News Online Magazine: RFID technology is sparking privacy concerns with the technology “moving from geeky future-gazing to a mainstream population,” BBC News Online Magazine reports. The British Medical Association has said that it would not raise an ethical objection to implanted RFID chips “as long as it was proven to be safe and there was no coercion,” BBC News Online Magazine reports (Coughlan, BBC News Online Magazine, 10/15). [21]
Opinion: Benefit of Implantable Microchip is Unclear
An opinion piece in eWeek on Thursday examined the medical value of an implantable radio frequency identification chip that the FDA approved this week. The chip does not contain any medical information and is similar to “lower-tech and vastly cheaper” identification products such as bracelets and cards, eWeek columnist M.L. Baker writes.
Applied Digital Solutions’ VeriChip, which was approved this week, contains a code that must be read by a $650 scanner to access a patient’s medical information. It costs between $150 and $200 to have the chip implanted, and the patient then pays $9.95 per month for a subscriber registry service (Baker, eWeek, 10/14). The company says VeriChip could improve health care and help avoid mistakes because doctors would know whom they were treating and have patients’ medical information (iHealthBeat, 10/14).
VeriChip, however, “suffers from the exact same problem that low-tech versions do: patients will be unwilling to pay for them, and providers won’t trust that patients will update their information,” Baker writes. The VeriChip database also may lack information such as whether a patient filled a prescription or reacted badly to a medication, which could be provided by “only the most sophisticated, up-to-date medical records,” according to Baker. Baker writes that the chip will just serve as another way to communicate information, and the information could actually be less comprehensive than a provider’s records.
However, Lorraine Fernandes, senior vice president of health care practice at data integration firm Initiate Systems, said she sees the chip as another way to facilitate patient identification, similar to other methods such as biometric identification (eWeek, 10/14).
A separate column in the Washington Post on Friday looked at the privacy concerns surrounding electronic tracking and data capture devices such as RFID chips in health care. It might be possible one day to mine information from such RFID chips or to conduct a customized Google search on the chips, according to the Post.
“It’s a whole new world. It’s sort of like all these little details about our lives are being recorded,” Internet security consultant Richard Smith said. “We love the conveniences. We love the services. But people kind of instinctively know there’s a dark side to this. They just hope it won’t happen to them”.[22]
Boston Hospitals Test RFID To Track Patients, Equipment
Several Boston hospitals are testing radio frequency identification tags to track critical medical equipment, the Boston Globe reports. Some local hospitals also are piloting programs using the technology to monitor patient wait times and to ensure that patients are given the correct medications or blood types.
Massachusetts General Hospital, which two years ago began using Radianse RFID technology in its operating room, this spring will roll out RFID technology in other departments and also will use the tags to label medicine and medical equipment. The hospital’s computer system will send alerts to staff members’ pagers to warn them of certain situations, such as if patients are about to be given the wrong medicine or if a patient waits more than 30 minutes between medical tests, the Globe reports. The hospital also this month will begin using RFID tags in its blood bank to ensure that transfusion recipients get the right blood type.
Beth Israel Deaconess Medical Center, which last fall began using RFID, worked with PanGo Networks to develop a system of small tags with transmitters that send signals to wall-mounted receivers, the Globe reports. The signals transmit to hospital computers the location of patients, surgeons and medical equipment.
Physicians and other officials at the Boston hospitals using RFID technology say they are concerned about patient privacy, so they are only using temporary, external tags hidden in standard identification bracelets, the Globe reports. The tags hold information such as a patient’s name, hospital identification number and blood type. However, privacy advocates are concerned that as RFID technology becomes standard in ensuring patient safety, it is less likely to be optional, the Globe reports.[23]
Beth Israel to Test RFID in Emergency Department
Beth Israel Deaconess Medical Center in Boston next month will begin a pilot program to track patients, medical records and equipment in the emergency department with radio frequency identification technology, Health-IT World News reports. The hospital hopes to improve workflow by identifying patterns in the ED and tracking how long people and supplies are in certain places, Beth Israel CIO John Halamka said.
The hospital is currently planning the pilot and conducting a survey throughout the facility to determine its specific RFID needs, Halamka said. Because of the complex nature of EDs, accurate tracking and getting wireless signals will be a challenge, he said. However, if the hospital can track equipment and people in individual ED rooms, the pilot will be successful, Halamka said.
Beth Israel is working with wireless firm SideBand Systems to determine the hospital’s RFID bandwidth and channel requirements. A PanGo Networks Web-based tracking system will monitor the tagged items and patients in the pilot. More than 100 ED workers will participate in the program (Berman, Health-IT World News, 6/29).
A recent survey of more than 350 IT executives found that requirements from government and large retailers have encouraged 46% of respondents to begin RFID adoption. Another 51% expect to deploy RFID within two years. The survey was conducted in April by BearingPoint, the Software & Information Industry Association and CIO magazine.[24]
Siemens Pilots RFID at New York Hospital
Siemens Business Services last week announced a pilot with New York’s Jacobi Medical Center to track patients using radio frequency identification technology, InfoWorld Daily News reports. Under the program, RFID chips will be placed in patients’ wristbands, and clinicians will use Wi-Fi-enabled Tablet PCs to read the data.
The wristband chips will contain the patient’s name, date of birth, gender and a medical record number that links to lab, billing and pharmacy information. The project is intended to improve access to medical records and reduce the risk of misidentifying patients. Most hospitals still use paper-based wristbands to identify patients.
A program in Mexico City has implanted RFID chips into patients with Alzheimer’s, diabetes and other chronic conditions for identification purposes (Schwartz, InfoWorld Daily News, 7/23).
In related news, a group of pharmaceutical companies this month began testing the use of RFID to track individual drug bottles from manufacturing plants to distributors to pharmacies. The program will run through September, when industry groups will evaluate and publish the results. The group of drug makers includes Abbott Laboratories, Johnson & Johnson, Pfizer and Procter & Gamble.[25]
MIT Lab to Study RFID in Health Care
Auto-ID Labs, the Massachusetts Institute of Technology group that helped develop radio frequency identification, this week announced the creation of the Healthcare Research Initiative, a project to study the use of RFID, mass serialization and sensing technology in health care, InformationWeek reports. Auto-ID hopes the research from the project will help the health care industry in its RFID implementation decisions.
Initially, the project will focus on the use of RFID for tracking drugs through the supply chain, from raw materials through the sale of drugs, InformationWeek reports. The project will look at issues such as whether RFID emissions affect pharmaceutical products. Auto-ID will confirm its findings with physical trials of its research.
The research will be conducted with EPCglobal, the organization supervising the development of RFID standards, and health care companies and industry associations.[26]
Atlanta Physicians Will Pilot Health Credit Cards
Atlanta will test a credit-card machine that will allow physicians to access information about a patient’s health benefits by swiping a card and then printing out the information, the Atlanta Business Chronicle reports. Financial transaction company First Data will launch the pilot in January.
The company is not the first to pilot such a project. Wyoming, North Dakota and Nevada have programs that use “smart cards” to store medical records, the Chronicle reports. First Data’s rival HealthTransaction Network also is encouraging insurance companies to issue debit cards that would connect to medical spending accounts.
First Data’s machine, made by Hypercom, will feature smart-chip technology and magnetic strips. The chips are not being tested in the pilot, but they allow more information to be transmitted and stored, the Chronicle reports. Once some privacy issues are resolved, the terminals will include the chips, which already have been used in Europe, said Beverly Kennedy, president of First Data’s health care division. The machines will plug into walls like credit-card terminals and will be easy to use, she said.
To minimize the risk for physicians, First Data will provide the terminals at no cost but will still collect transaction fees since it owns the network that carries the data, the Chronicle reports. The terminals will first be tested in doctors’ offices and will offer only eligibility data. Insurance companies taking part in the program will issue their customers special cards for use at participating health care facilities. Blue Cross Blue Shield of Georgia, one of the largest insurers in the state, might participate, the Chronicle reports.
Officials plan to eventually broaden the program on a national level to opticians and dentists and to offer comprehensive medical information including referrals, authorization and claims status. They also hope the system will cut health care administration costs, which stand at $275 billion a year.[27]
References
[1] iHealth beat Nov 22, 2005 (Colliver, San Francisco Chronicle, 11/22/2005) [2] Health-IT World News, 9/27/2005 [3] BMJ, 7/17/2005 [4] E-Health Insider, 6/1/2004 [5]Glover, Pittsburgh Business Times, 5/24/2002 [6]Jordon, Omaha World-Herald, 10/8/2003 [7] Circelli, 5/15/2002 [8] Electronic Government: Progress in Promoting Adoption of Smart Card Technology,” January 2003 [9] Merritt, Electronic Engineering Times, 9/22/2003 [10] Blue Cross press release, 1/29/2004 [11] Crane, Wall Street Journal, 11/10/2005 [12] Rubenstein, Wall Street Journal, 7/26/2005 [13] Mulder, Syracuse Post-Standard, 6/4/2004 [14] San Jose Mercury News, 8/5/2004 [15] Rubner, Atlanta Business Chronicle, 11/5/2004 [16] E-Health Insider, 8/17/2004 [17] Healthcare IT News, 09/13/2005 [18] Weiner, “Marketplace,” APM, 9/5/2005 [19] Glover, Red Nova/The Business, 7/31/2005 [20] Gladstone, San Jose Mercury News, 8/26/2004 [21] iHealth Beat, 10/20/2004 [22] O’Harrow, Washington Post, 10/15/2004 [23] Berdik, Boston Globe, 2/1/2005 [24] Repsher Emery, Washington Technology, 6/29/2004 [25] Whiting, InformationWeek, 7/26/2004 [26] Whiting, InformationWeek, 5/4/2004 [27] Rubner, Atlanta Business Chronicle, 11/5/2004